As mentioned in my post of January 31,
there are many studies showing a correlation between Adverse Childhood Experiences (ACE's) and a wide variety of
psychiatric and physical conditions. This is probably also true of the effects
on offspring of certain parental behavior problems.
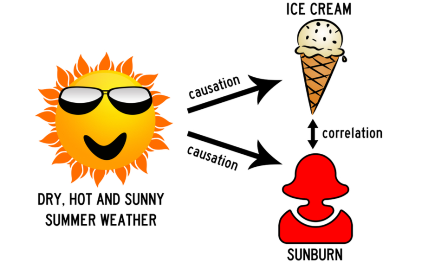
Correlation does not mean causation. Answering
the question of whether two characteristics that correlate are also involved in
a causative relationship depends on a number of factors. How strong is the
correlation? A weak correlation can be a statistical fluke, If there is a lot
of natural variation in the characteristics being discussed, the found
relationship may just be a coincidence.
Are there other variables that are not
controlled for that create the correlation?
In order to verify any relationship seemingly uncovered in any given
study, repeated experiments that lead to the same result become necessary. And even
if causation is involved, we may not know which variable was the causative
factor and which the result.
The metrics I tend to use also include
my answers to the following questions: If A and B are indeed causally related,
what else would I have to believe? Can I think of a third, uncontrolled-for
variable that could account for both A and B? Can I come up with any logical and
known facts or data that might be the explanation for an apparent causative
relationship, or does it seem inexplicable or even off the wall?
Last, is this result consistent with
what I have seen clinically in my 40 plus years as a psychiatrist, or does it fly
in the face of it? Now here it is possible that I might be looking at only confirmatory
evidence of my opinions and discounting disconfirming evidence (confirmation bias), although I like to
think I have at least a modicum of objectivity.
So I also ask other psychiatrists
and therapists if they’ve seen the same things I have in their clinical
experience. When I do that, I have to take into account that I asked my patients a lot of
questions that most therapists never even think about asking – for example, “What
does your mother-in-law think about this problem your daughter is having?” So
they might or might not be able to give me any relevant information.
Many studies showing the same thing
makes for a stronger case for causation. When it comes to ACE’s and later illnesses, both psychological and physical, they
usually pass most if not all of the tests above with flying colors. And they keep
on coming in. Here’s some recent additions:
1. Childhood Adversity Tied to Race-Related Differences in
Brain Development
In this study,
exposure to trauma was linked to lower gray matter volume in key brain regions
in black kids. Among children ages 9 to 10 years, white kids showed
greater gray matter volumes compared with black kids in the amygdala,
hippocampus, frontal pole, superior frontal gyrus, rostral anterior cingulate,
pars opercularis, pars orbitalis, lateral orbitofrontal cortex, caudal middle
frontal gyrus, and caudal anterior cingulate (all p<0.001).
Compared with
white children, black children had experienced more traumatic events, material
hardship, and family conflict and lived in more disadvantaged neighborhoods,
while their parents/caregivers had lower income and educational attainment and
were more likely to be unemployed.
This
analysis provides evidence that contradicts claims about inherent race-related
differences found in the brain.
Dumornay N.M., et. al., "Racial
disparities in adversity during childhood and the false appearance of
race-related differences in brain structure." Am J Psychiatry 2023
2.
Childhood Adversity Tied to CVD in Early Adulthood
Children who experience adversity ― including serious family illness or death, poverty,
neglect, or dysfunctional and stressful family relationships ― are at increased risk of developing cardiovascular
disease (CVD) in early adulthood, a large Danish study of patients aged 16 – 38
has found. Compared to young adults who experienced little adversity in
childhood, peers who experienced high levels of childhood adversity had about a
60% higher risk of developing CVD, the researchers found.
Bengtsson
J. et al. “Childhood
adversity and cardiovascular disease in early adulthood: a Danish cohort study.”
Eur Heart J. 2023 Feb 14;44(7).
3.
Adolescents’ positive perceptions
of their relationships with both their parents are associated with a wide range
of favorable outcomes in young adulthood.
In this study of more than 15,000 adolescents, higher levels of adolescent-reported
parental warmth, parent-adolescent communication, time together, academic
expectations, relationship and communication satisfaction, and maternal
inductive discipline were all associated with favorable outcomes in young
adulthood.
Participants rated their depression,
stress, optimism, nicotine dependence, substance abuse symptoms (alcohol,
cannabis, or other drugs), unintended pregnancy, romantic relationship quality,
physical violence, and alcohol-related injury.
This was done while controlling
for age, biological sex, race and ethnicity, parental educational level, family
structure, and child maltreatment experiences.
Ford, et. al. “Associations Between Mother-Adolescent and
Father-Adolescent Relationships and Young Adult Health.” JAMA Netw Open. 2023;6(3)